The 2024 Catheter Ablation for AFib Guidelines- what's new?
I analysed the 2023 Atrial Fibrillation Guidelines only a few months ago, especially how they strengthened their recommendations for invasive treatment of AF in heart failure patients. And hot on its heels, we have another big drop this week, as the 2024 Catheter Ablation for AF Guidelines has just been published.
This latest document was an International collaboration drawing in global expertise from the USA, Asia, Europe and our AFHF & AFFU-AW studies Principal Investigator Prof Richard Schilling from the UK as well. The full document is 107 pages long and refers to 1,467 other articles in it. 🤯 Each recommendation made had to be supported by at least 80% of the expert writing committee to be included in this consensus document.

Now the last Catheter Ablation Guidelines were published in 2017 and have been referenced by other scientific papers 2589 times! But seven years in the Catheter Ablation space feels like 14 and so a revised expert consensus was needed to reflect and incorporate all the developments in the space since then. In this article, we are going to highlight five important changes and to be aware of.
1. There’s a new type of AF
AF has traditionally been categorised based on it’s duration.
Paroxysmal AF is the term for repeated episodes that last more than 30 seconds but less than 7 days- either terminating spontaneously or with intervention.
Persistent AF is the term for AF that has been continuous for more than 7 days.
The 2017 Guideline writers were the first to divide persistent AF into ‘early Persistent AF’ for continuous episodes lasting between 7 days and 3 months and ‘long-standing persistent AF’- for continuous episodes lasting more than one year.
The 2024 Guideline writers have gone one step further to divide Paroxysmal AF into early Paroxysmal AF for episodes lasting between 30 seconds and 24 hours only.
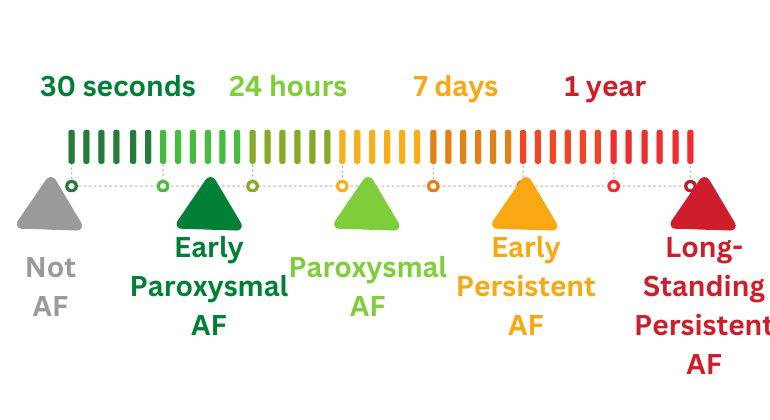
These sub-divisions may seem arbitrary but the division was made because the authors believe the structure and electrical properties change after 24 hours in AF. Also the risk of hospitalisation and stroke is greater for a 24-hour episode. In reality, AF is probably closer to a continuous spectrum and the primary benefit of this type of classification is to standardise communications about AF between different professionals and when describing study populations in research.
2. More discussions on Catheter Ablation of Asymptomatic AF
In 2017, the rationale for Catheter Ablation of asymptomatic AF was weak. It was given a class II (lowest), level of evidence B recommendation stating that it ‘may be considered in selected patients’. I went into the differences between asymptomatic and symptomatic AF here.
There was more discussion about it this in the 2024 Guidelines- although the evidence was not strong enough to change the recommendation. The writers stressed the importance of considering ‘pseudo-asymptomatic’ AF status- a fancy way of saying AF with symptoms that are not appreciated until the AF is removed and the patient feels much better.
They suggested in younger patients, a cardioversion may be an effective way to restore normal rhythm and compare whether the AF was truly asymptomatic. The authors also refer to studies that show catheter ablation can slow the progression of AF. They don’t refer to the EAST-AFNET6 study which suggested early restoration of rhythm control may improve survival- but this was a symptomatic group of patients so they are appropriately cautious to not translate any implications from this study across.
So in the Guidelines, the authors call this an ‘Area of Uncertainty’ in 2024. Although it may be reasonable in selected patients, the decision must be reached after a thoughtful conversation about the risks and potential benefits. Maybe this will be something we will know more about in the next Guidelines.
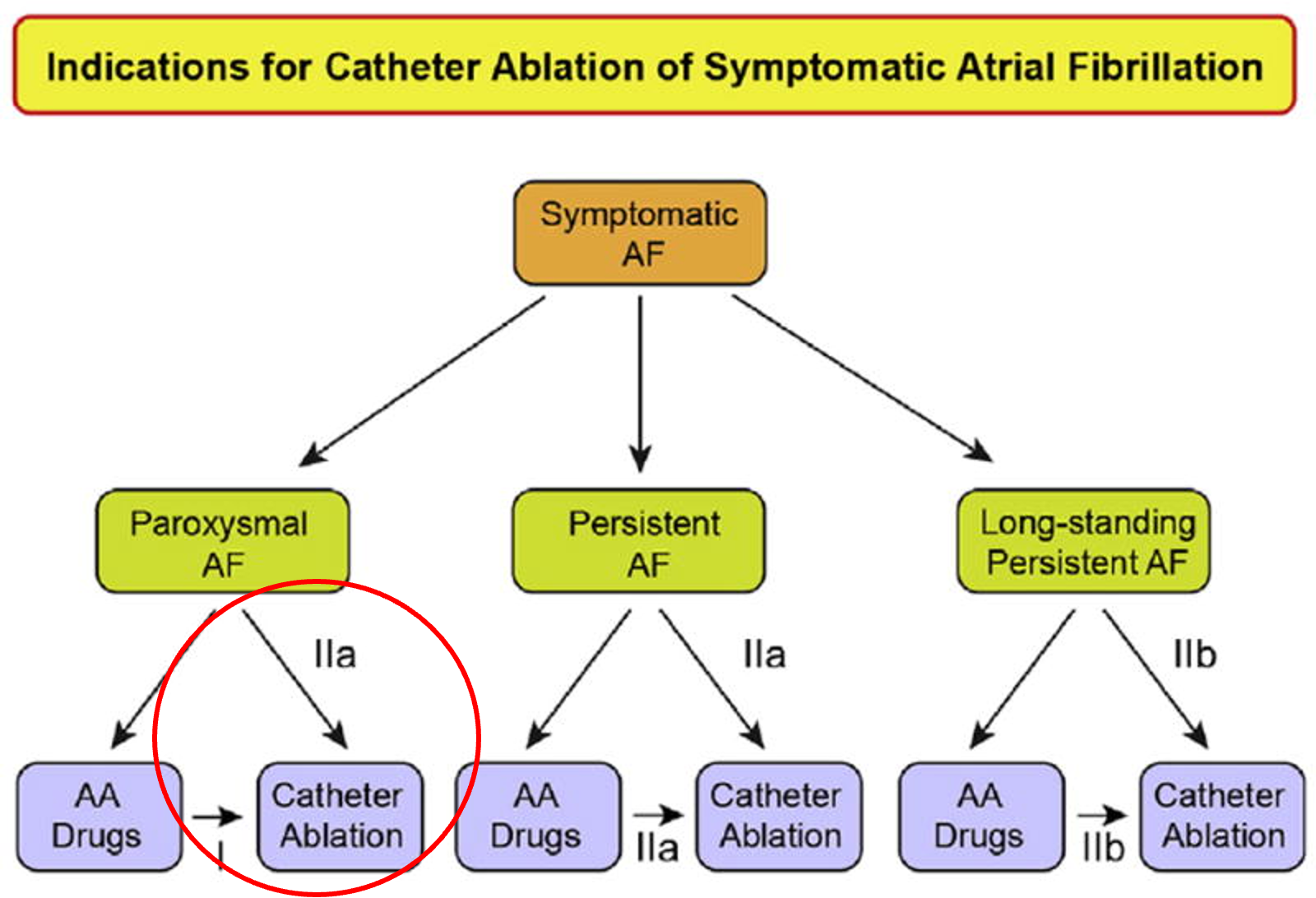
3. A stronger vote for Catheter ablation in intermittent AF

In 2017, Catheter Ablation was considered reasonable to do in patients with symptomatic and intermittent (paroxysmal) AF before the trial of medications. The language in the 2024 Guidelines has been upgraded as “Advice to DO”- meaning the authors recommend the use of Catheter Ablation as the first line in patients with this early phase. Ofcourse, the decision for Catheter ablation instead of drugs should still follow a conversation with a physician about the potential risks:benefits of both- but it is now reasonable to proceed to Catheter Ablation without a trial of anti-arrhythmic tablets first. This recommendation was likely driven by strong, randomised controlled trial evidence in the past few years demonstrating the superior efficacy in achieving freedom from AF in randomised controlled trials.
Catheter Ablation remains the first line treatment for patients with symptomatic AF who have trialled and not tolerated or responded to an anti-arrhythmic drug.
Catheter Ablation is the first line treatment for AF in the setting of Heart Failure with reduced heart function believed to be caused by the AF. We have spoken about this before in depth so we won’t cover this much further here. The authors give some suggestions on how a physician can try to determine if the AF is caused by the AF- either by looking at features on their ECG, Echo scan or MRI scan.
It is reasonable to use the same considerations in patients over 75 years old, suggesting age alone should not be a discriminating factor.
Catheter ablation should be considered in patients with a heart condition called Hypertrophic Cardiomyopathy. We discuss here why this sub-category of patients require special considerations and how this is at odds with the current UK guidelines.
4. Pulsed Field Ablation
The authors did not recommend one type of ablation over the other but did go into depth about the evidence and advantages behind radio-frequency ablation, cryo-balloon ablation, laser ablation and, for the first time, pulsed-field ablation- the new technology not available in 2017.
The authors recognise the overwhelming evidence behind the pulmonary vein isolation technique, which can be delivered with any of these technologies and should be a greater priority than the type of technology used.
However, the Guideline was a good summary of the evidence behind this new, emerging technology. The authors discuss the potential advantages in terms of the quality of the ablation treatment that can be delivered (in theory) with Pulsed Field ablation and also the potential safety benefits over the other technologies because it is heart-tissue selective. However, this is tempered by their recognition that in the latest randomised trial of Pulsed Field Ablation vs the other technologies, no benefit was shown and that a number of trials are still ongoing to test and compare it in different settings. So this is likely another question that will probably be deferred till the next Guidelines.
5. A shorter Blanking period
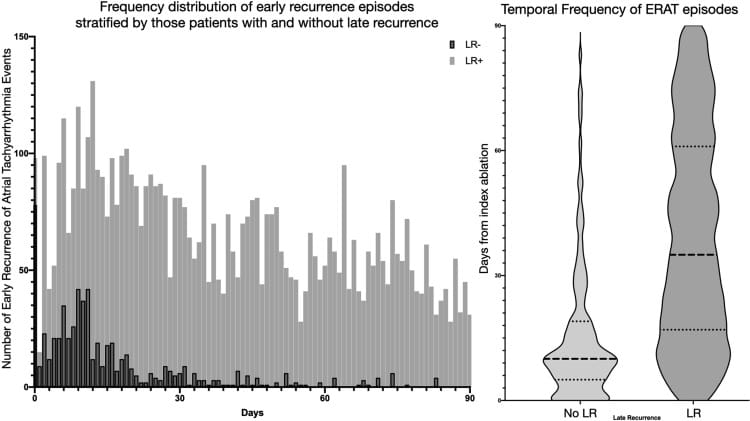
The blanking period is the name traditionally given to the three months after a Catheter Ablation procedure wherein episodes of AF that occur, are not considered ‘procedural failures. This is because they may reflect inflammation caused by the ablation itself or occur whilst the ablation lesions themselves mature to the full extent.
From a research perspective, they are also important when evaluating the efficacy of an ablation treatment or protocol as episodes during this period should not be counted as recurrences or treatment failures.
From a patient perspective, this is important because it can provide some reassurance as these ‘blanking period AF episodes’ can be common and without pre-warning, they can cause anxiety that their procedure has not worked.
However, this means that the decisions about repeat ablation procedures or any further treatments may be put on hold till the end of the blanking period. For some patients this means three months of debilitating AF symptoms till further interventions can even be considered.
And so the authors evaluated whether a three-month window was really justified. They reviewed data from studies using implantable loop recorders to monitor AF episodes during the blanking period and whether they were related to further episodes after the blanking period (i.e. whether they were temporary episodes that will settle spontaneously or whether they will continue after the 3-month point and thus warrant consideration of further treatments).
Episodes that occured in the first month were more likely to settle down spontaneously whereas episodes that continue into the third month were unlikely to resolve on their own and likely represented true ‘AF recurrence’ that need evaluation. And so the 2024 guidelines recommend a shortened blanking period of 8-weeks only. Therefore patients with recurrences from 8 to 12 weeks who would traditionally be told to watch and wait for another month, should now be considered for further AF treatments at an earlier time point. This will also change the way studies report ablation failure/success.
Summary
It is important to remember the number one rule of this blog- No two individuals with AF are the same. And so these recommendations and Guidelines are sweeping generalisations and should not be directly considered in isolation. There are exceptions to each one and they reflect a summary of a very simple voting system based on a diverse set of trials that are continuously evolving.
There is no technological superiority of one catheter over another and it is important to deeply understand the risks and benefits of the invasive procedure before undertaking it with realistic expectations for the likelihood of success on an individual level as well.
The 2024 Guideline: Tzeis S, Gerstenfeld EP, Kalman J, Saad EB, Sepehri Shamloo A, Andrade JG, Barbhaiya CR, Baykaner T, Boveda S, Calkins H, Chan NY, Chen M, Chen SA, Dagres N, Damiano RJ, De Potter T, Deisenhofer I, Derval N, Di Biase L, Duytschaever M, Dyrda K, Hindricks G, Hocini M, Kim YH, la Meir M, Merino JL, Michaud GF, Natale A, Nault I, Nava S, Nitta T, O'Neill M, Pak HN, Piccini JP, Pürerfellner H, Reichlin T, Saenz LC, Sanders P, Schilling R, Schmidt B, Supple GE, Thomas KL, Tondo C, Verma A, Wan EY, Steven D, Agbayani MJ, Jared Bunch T, Chugh A, Díaz JC, Freeman JV, Hardy CA, Heidbuchel H, Johar S, Linz D, Maesen B, Noseworthy PA, Oh S, Porta-Sanchez A, Potpara T, Rodriguez-Diez G, Sacher F, Suwalski P, Trines SA. 2024 European Heart Rhythm Association/Heart Rhythm Society/Asia Pacific Heart Rhythm Society/Latin American Heart Rhythm Society expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2024 Mar 30;26(4):euae043. doi: 10.1093/europace/euae043. PMID: 38587017; PMCID: PMC11000153.
