Atrial Fibrillation and Chest Pain
How can an irregular heart rhythm cause chest pain? And can it lead to a heart attack?
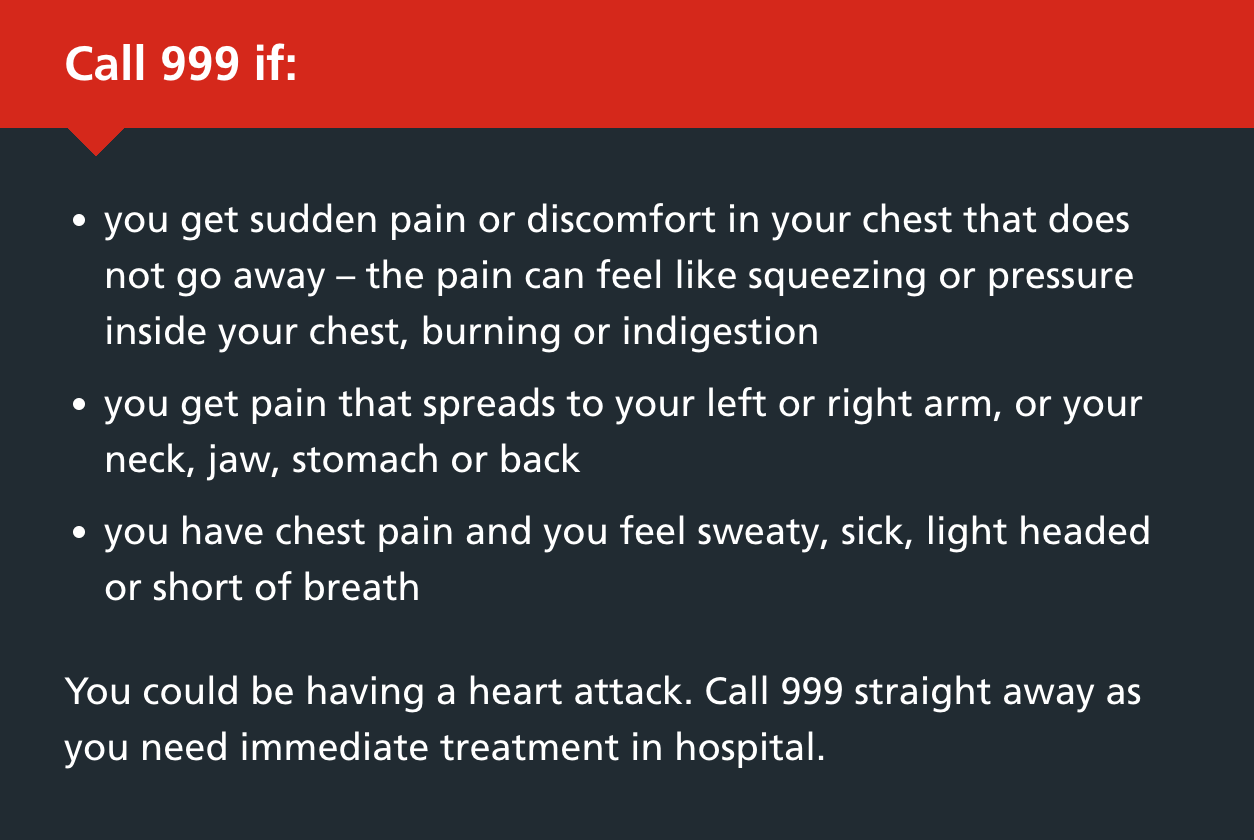
Chest pain is a concerning symptom to a Cardiologist. Guidelines from the NHS in the UK and the American Heart Association advise the same thing- call 999🇬🇧 (or 911🇺🇸) if you are concerned it may be a heart attack. And this makes the management of atrial fibrillation incredibly challenging as it can precipitate chest pain symptoms, leaving patients understandably very worried.
How common is Chest pain?
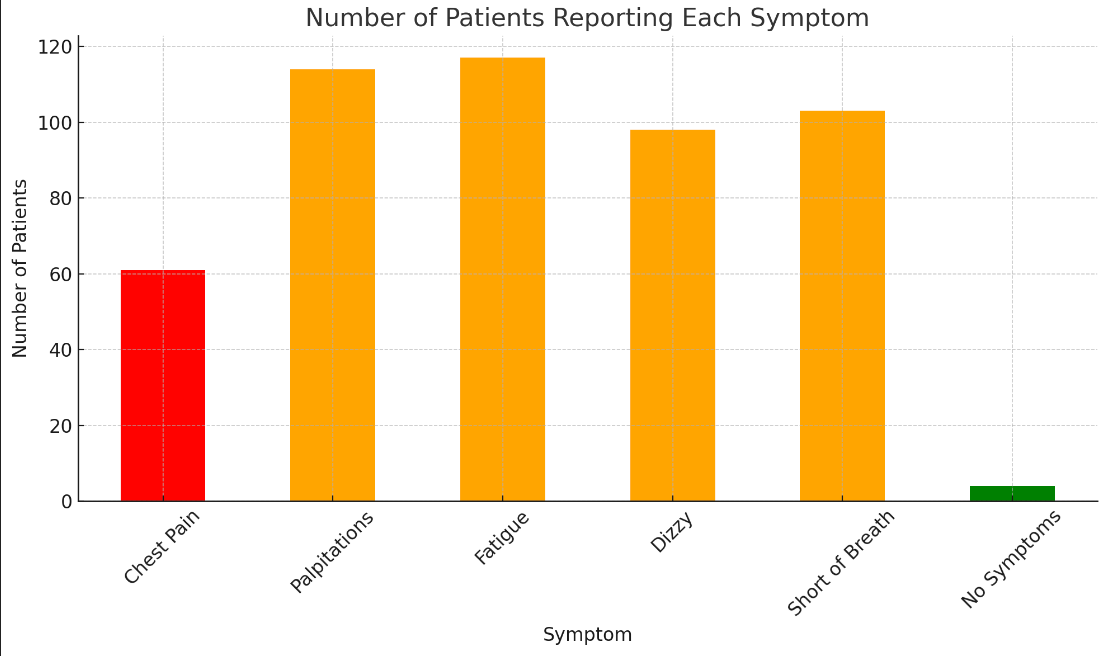
Not all patients with AF will experience chest pain, in fact, it is less commonly reported than palpitations, fatigue or shortness of breath.
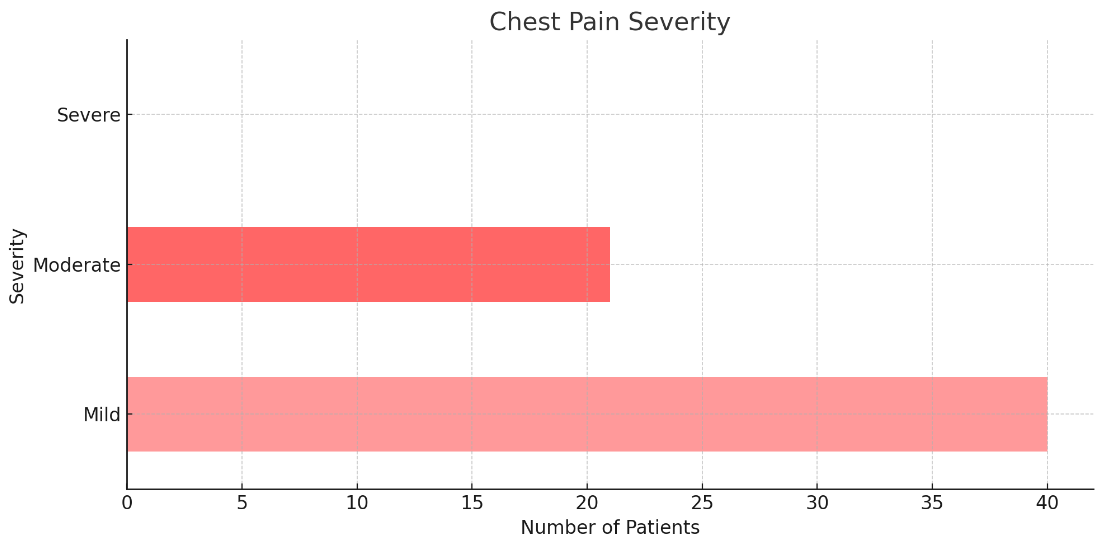
These results have not been formally published yet, but in the AFFU-AW study, we see a similar picture in patients with AF before they undergo catheter ablation. Palpitations, shortness of breath and fatigue are most common. Chest pain is seen, but to a lesser extent. When it is reported it is usually mild, sometimes moderate in severity.
But why does it cause chest pain?
There are several possible explanations. The first scenario is that AF may not be causing the chest pain… the chest pain may be causing the AF. During a heart attack, the reduction in blood supply, the imbalance in hormones and the stress response may all precipitate the onset of AF. This is why it is so important to not ignore chest pains, especially if it is not a typical symptom for your AF or if you have not had it before. One small analysis of 57 patients with chest pain and Atrial Fibrillation presenting to A&E and admitted to a hospital in Israel, found coronary artery disease in 42%. They found the description of the nature of the pain did not help differentiate patients with underlying coronary disease from those who did not.
And so to re-iterate the advice from the NHS and American Heart Association, if you experience chest pain or having any symptom that you think may be a heart attack, do not delay calling for medical help as every minute counts.
Although a heart attack can cause AF, AF itself does not cause a heart attack. Even when it causes the heart to beat very fast. A heart attack is when a coronary plaque (the cholesterol-filled, fatty collections inside the coronary arteries) ruptures and blocks the vessel. AF does not cause this. But AF does alter the blood supply to the heart and this can lead to angina-type chest pains.
Greek researchers in a 2002 study measured the effect of the onset of Atrial Fibrillation on coronary blood flow by passing a very small catheter that was able to measure flow rate whilst patients were in normal rhythm and then after triggering AF. They reported the rate of coronary flow increased (because of the increase in heart rate). However the oxygen demand of the heart increased to a greater extent and so the oxygen mismatch was greater i.e. the supply increased, but the demand increased by a greater extent so the net deficit was larger.
For individuals with existing plaques and coronary artery disease, the likelihood of chest pain sensations is more likely as the additional strain of AF and faster heart rates on top of their narrowed arteries are more likely to lead to insufficiency of coronary blood flow. This may be one reason why slowing the AF rate down with medicines like beta-blockers or calcium channel blockers can improve symptoms.
But why does it only affect some people?
I want to share another really interesting study. It is a small study of 30 patients so it should be considered as ‘thought-provoking’ more than anything else. The Swedish investigators invited patients with permanent AF who were classified as symptomatic of their AF or asymptomatic based on their scores on a symptom questionnaire.
Symptomatic patients had a lower pain threshold when assessed by pressure on the shin and the sternum than asymptomatic patients. Whether this may be due to a pre-existing hypersensitivity or even induced by their AF type was unclear but it warrants further investigation.
Chest pain after Catheter Ablation
This is a very specific circumstance that I want to cover. During the 24-72 hours after Catheter ablation, patients are advised to report any concerning symptoms including worsening chest pain.
This is because a degree of chest pain is to be expected- you have just had your heart instrumented and a treatment applied to the inside and so there will be residual effects that will cause some discomfort for most patients. However, this sensation should be reduced with time. Catheter ablation can also irritate the lining around the heart leading to inflammation, known as pericarditis. A review of the 2215 patients undergoing catheter ablation at the Cleveland Clinic in Ohio reported suspected, and treated for, pericarditis in more than 10% of their patients. The rarest outcome, but also the most serious, is chest pain due to a pericardial effusion (blood leaking into the sac around the heart). It is exceptionally rare for this to not be picked up during the post-procedure checks before discharge but it can happen and is the reason patients are advised to report back for medical attention if they experience new or worsening chest pain after their ablation procedure.
As a penultimate note, I want to reiterate once more: please don’t interpret this article as medical advice in any way- chest pain should always be taken seriously and if you are concerned it may be a heart attack, timing is important and so do not delay seeking medical advice.
And finally: to all our new subscribers- welcome! Every week, I try to cover a question someone from our studies asks or new developments in AF research and the implications. If you have a question or topic you would like me to cover please send me an email (nikhil@bartsaf.com). But please note- these articles should not be considered medical advice. Thank you for subscribing and please share it with anyone you know with (or interested in) Atrial Fibrillation. 🙏
References:
Chest pain/AF in A&E: Perelshtein Brezinov O, Vorotilina N, Vasilenko L, Kogan Y, Lev EI, Laish-Farkash A. Coronary artery disease among patients admitted with atrial fibrillation and chest pain. Coron Artery Dis. 2023 Mar 1;34(2):96-101. doi: 10.1097/MCA.0000000000001206. Epub 2022 Dec 13. PMID: 36515228.
Coronary blood flow in AF: Kochiadakis GE, Skalidis EI, Kalebubas MD, Igoumenidis NE, Chrysostomakis SI, Kanoupakis EM, Simantirakis EN, Vardas PE. Effect of acute atrial fibrillation on phasic coronary blood flow pattern and flow reserve in humans. Eur Heart J. 2002 May;23(9):734-41. doi: 10.1053/euhj.2001.2894. PMID: 11978000.
Pain sensitisation in AF: Jackson A, Frobert O, Boye Larsen D, Arendt-Nielsen L, Björkenheim A. Patients with symptomatic permanent atrial fibrillation show quantitative signs of pain sensitisation. Open Heart. 2021 Jun;8(1):e001699. doi: 10.1136/openhrt-2021-001699. PMID: 34140311; PMCID: PMC8212408.
Post-ablation pericarditis: Nakhla S, Mentias A, Rymer C, Hussein A, Wazni O, Rickard J, Baranowski B, Cantillon D, Klein AL, Cremer PC, Taigen TL. Acute pericarditis after atrial fibrillation ablation: Incidence, characteristics, and risk factors. Heart Rhythm O2. 2022 Feb 13;3(3):248-251. doi: 10.1016/j.hroo.2022.02.008. PMID: 35734298; PMCID: PMC9207724.
