Ear stimulation: A new approach to AFib treatment
We need more treatment options for AF. Despite the effectiveness of anti-arrhythmic drugs and catheter ablation, we still need additional treatment options for patients. A wider choice of treatment strategies would allow us to match the right treatment to the right patient and AF profile.
And so it was refreshing to read the results of the TREAT-AF trial and the ‘neuromodulation’ strategy; demonstrating an entirely different approach to AF management. Now there is good rationale and science behind stimulation of the ear for AF management, so please read on before making your judgement…
AF and the autonomic nervous system
The link between the heart and brain is not new. We know that nerves connect the two vital organs and we see the effect on them during an ablation procedure. The ‘Vagal nerve’ provides a counterbalance, on the heart and the rest of the body, to the pro-stimulant ‘fight or flight’ effect of the sympathetic nervous system. An overactive sympathetic nervous system can increase the risk of arrhythmias like AF. So an attractive hypothesis is that activating the vagal nerve might suppress the sympathetic nervous system and thus reduce the risk of AF episodes.
However, there isn’t a tablet that directly activates the vagal nerve and implanting something into the body to stimulate the vagal nerve along its path from brain to heart is a highly invasive approach. This is done for some severe cases of epilepsy so we have evidence of very good safety from these studies.
Vagal stimulation and post-operative AFib
The most direct way to stimulate the vagal nerve is by directly applying an electric current to it. However, this requires surgery to open the chest. Therefore one approach to study the effect on AFib was to test it in patients who are already having heart surgery for other reasons. Researchers in Oklahoma tested the effects of direct Vagal Nerve Stimulation in patients undergoing heart surgery by connecting a stimulator wire to the vagal nerve during the operation. Half the patients had Vagal Nerve Stimulation (the active study group) applied for 72 hours and half had the wire connected but no stimulation delivered (the sham placebo group).
AFib is commonly seen in patients after cardiac surgery. The handling of the heart leaves it irritable and the emergence of AFib can slow down recovery and is associated with worse outcomes. So if the likelihood ofpost-operative AFib can be reduced it may lead to faster recoveries.

This was a small study of 54 patients only but the effects were clear- the active study group had a significantly lower rate of AFib events in the post-operative period- 12% rather than 36% seen in the sham placebo group.
Although the surgeons implanting the wire were able to see where they were placing the stimulator wire, identifying the vagal nerve and where best to activate it, is challenging and hard to get right. Also, there were no additional risks reported for the surgical placement of the stimulator wire in patients who needed heart surgery anyway. It would be hard to justify taking on the risks of surgical placement purely for the purpose of vagal nerve stimulation
A safe, non-invasive approach to vagal nerve stimulation
Fortunately, there is a way that the vagal nerve can be targeted without any needles or incisions. A small branch of the vagus nerve lies just beneath the surface of the ear.
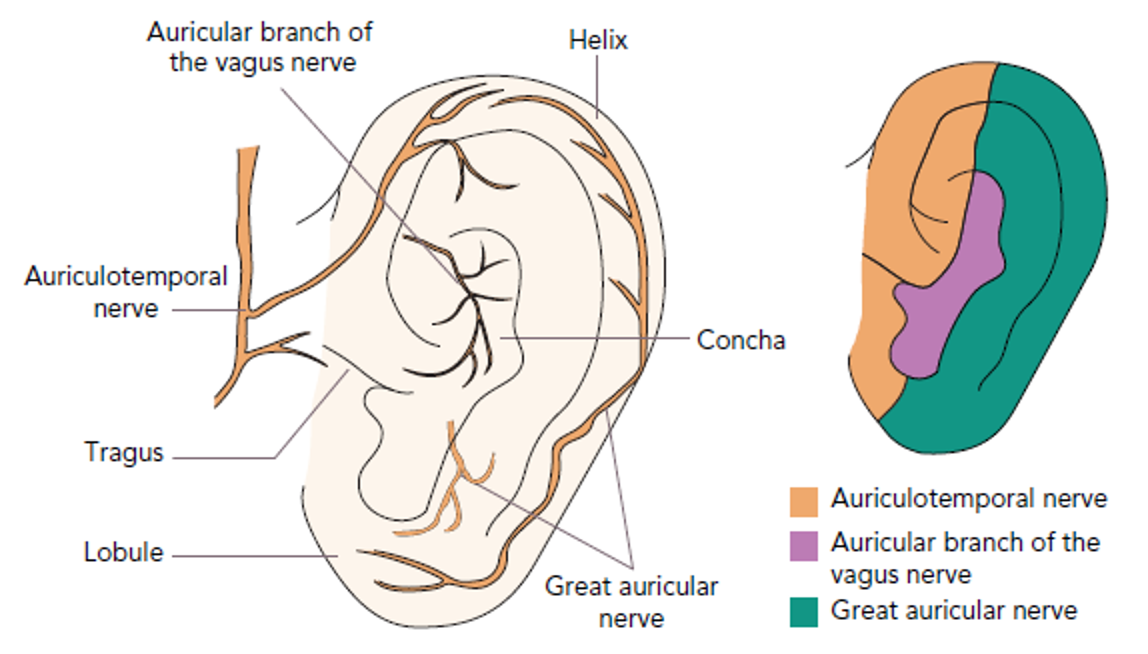
Studies performed in patients with epilepsy have shown the vagal nerve can successfully be activated by connecting a TENS machine that delivers electrical pulsations to the ear. The ‘auricular branch of the vagal nerve supplies the central section of the ear in most people. Stimulation of this nerve sends signals to the brain which coordinates the vagal nerve effect onto the heart.
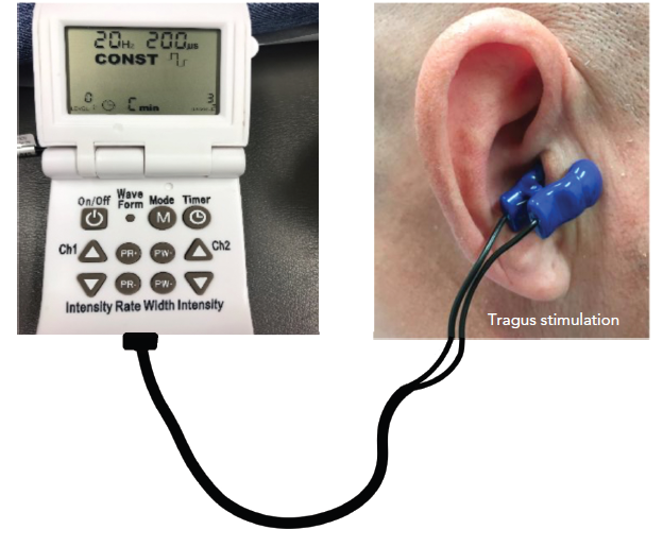
There are dedicated devices that can safely deliver stimulation in a controlled manner. The dose can be gradually increased up till a vibration or pulsation sensation is felt that delivers the effect. So there is no fixed level or dose for vagal nerve stimulation- the threshold are very personal depending on individual tolerance. There also isn’t a strict protocol for how long you need to wear it for. The studied protocol uses a regimen of one-hour per day, with the user free to do their normal activities at home whilst wearing the ear clip.
The TREAT-AF Study
On the back of the post-operative AF data, the cardiac researchers at Oklahoma decided to test the effect of non-invasive Vagal stimulation on AFib.
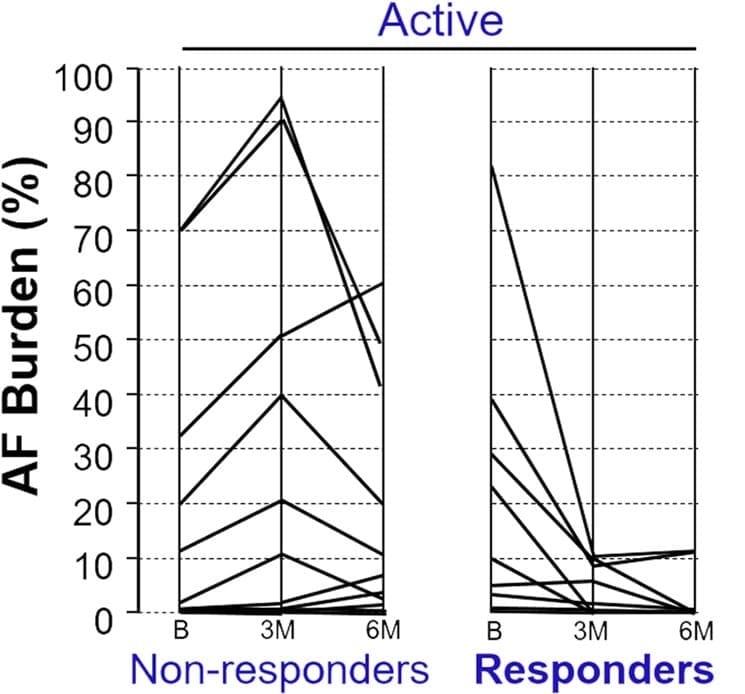
They recruited 53 patients, half received Tragus stimulation and half received a sham placebo treatment. Patients in the active group had a greater reduction in their AF burden after 6-months of treatment than patients who received the placebo sham treatment. The active group had an average reduction of 75% in their AF burden, whereas there was no significant change in the sham placebo group. This equated to an 85% lower AF burden after treatment in the active group compared to the placebo group.
The researchers also measured blood tests that suggested Tragus nerve stimulation reduced the amount of inflammation in the body, which may be an additional mechanism of action.
The Vagal sweet spot
This approach won’t work for everybody. Everyone has their own balance of sympathetic and vagal nerve effects. In some patients, vagal nerve activation can be the trigger of their AF events. Studies of high-level vagal nerve stimulation in animals have show that it can lead to excessive slowing of the heart rate with a reduction in the heart’s threshold for AF events i.e. at risk of more AF events.
Individual response also varied considerably amongst the patients who received tragus stimulation too. Although the average AF burden was lower in the active group compared to the sham group. The active group could be split into responders and non-responders. Perhaps the anatomy in some patients varies, meaning their vagus nerve can’t be modulated via the ear or perhaps some patients simply don’t respond to vagal stimulation- further analyses of larger groups are needed to tease this out.
The TREAT-AF study enrolled patients with paroxysmal AF, with a median AF burden before treatment of 1.0-4.5%- roughly 2-8 hours of AF per week.
The mechanisms of triggering an AF event and sustaining an AF event are different. And we do not know the effect of tragus stimulation on patients with persistent AF. A quick look at the global database of ongoing clinical trials reveals that there are many studies ongoing in patients with high blood pressure, heart attacks, heart failure and ectopic beats.
An hour of application per day is also not insignificant. It may not have the side effects or risks of catheter ablation but this is still asking a patient to make a commitment of their time which again, may appeal to some patients, but not all.
Summary
We need more treatment options for AF. The safety profile of Tragus stimulation is really attractive but we need to better understand which patients will benefit from this and what the long-term effects are before using it for clinical treatments.
In particular, there are two scenarios that I would like to see studied:
- for patients with very early AF- individuals who have had their first episode or hospitalisation. If Vagal Nerve Stimulation, as part of a risk factor control programme (combined with weight loss, blood pressure control, and alcohol reduction) can we slow the rate of progression and potentially defer the need for medications or ablation?
- for patients with symptom recurrence after AF ablation- if a patient gets ectopics or even an AF recurrence after their ablation procedure, would vagal nerve stimulation reduce the number of onward events and symptoms?
But it is great to see innovation and originality in the AF space. Better drugs and catheter ablation approaches are still needed, but so are alternative evidence-based therapies.
References:
The Post-op Vagal Nerve stimulation study: Stavrakis S, Humphrey MB, Scherlag B, Iftikhar O, Parwani P, Abbas M, Filiberti A, Fleming C, Hu Y, Garabelli P, McUnu A, Peyton M, Po SS. Low-Level Vagus Nerve Stimulation Suppresses Post-Operative Atrial Fibrillation and Inflammation: A Randomized Study. JACC Clin Electrophysiol. 2017 Sep;3(9):929-938. doi: 10.1016/j.jacep.2017.02.019. Epub 2017 May 30. PMID: 29759717.
The TREAT-AF study: Stavrakis S, Stoner JA, Humphrey MB, Morris L, Filiberti A, Reynolds JC, Elkholey K, Javed I, Twidale N, Riha P, Varahan S, Scherlag BJ, Jackman WM, Dasari TW, Po SS. TREAT AF (Transcutaneous Electrical Vagus Nerve Stimulation to Suppress Atrial Fibrillation): A Randomized Clinical Trial. JACC Clin Electrophysiol. 2020 Mar;6(3):282-291. doi: 10.1016/j.jacep.2019.11.008. Epub 2020 Jan 29. PMID: 32192678; PMCID: PMC7100921.
