AFib in older adults
I want to acknowledge that older adults form a diverse group that I am bracketing together- ranging from fit, active octogenarians to frail individuals with multiple health conditions. Given this variability, you could question the value of categorising AF management based solely on age. Yet, certain physiological changes are inevitable with aging, influencing the prevalence, experience, and management of atrial fibrillation (AF). We must also recognise that most of our evidence-based recommendations are derived from younger populations, which highlights the need for a focused review of the nuances in AF management in older adults.
Why AF Is More Common in Older Adults
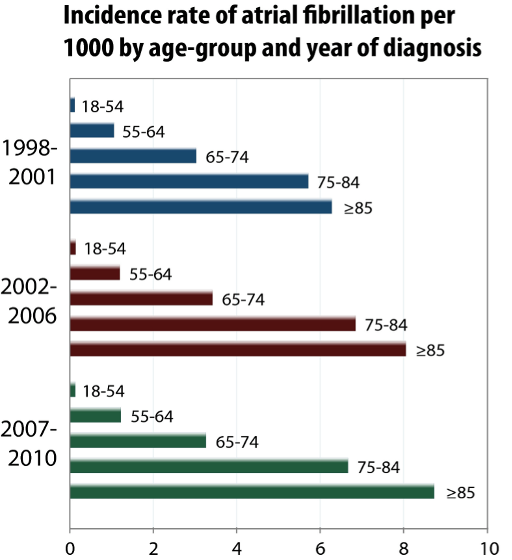
Age is the primary risk factor for AF and the likelihood of having the arrhythmia increases dramatically as we age.
Data from the American Heart Association underscores this:
- 80% of AF patients are over 65.
- AF prevalence exceeds 10% in individuals aged over 80.
- Frailty is present in 40-50% of older adults with AF.
European data, last updated in 2013 reported similar AF prevalences at 24.2% in men and 16.1% in women over 85.
Its prevalence increases significantly due to the structural and electrical changes in the aging heart:
- Atrial Fibrosis: Increased collagen deposition disrupts electrical pathways, creating conditions ideal for AF.
- Atrial Enlargement: Often resulting from chronic hypertension, left atrial enlargement increases AF risk.
- Electrical Conduction Changes: Collagen deposition and amyloid infiltration impair cardiac conduction, facilitating arrhythmias.
Limitations of Current Guidelines and Trials
Clinical trials for AF, especially invasive treatments primarily include younger patients (typically under 70 years old). Major studies that have been recently published around AF ablation that have been incorporated into contemporary guidelines such as Early AF, ADVENT, and CABANA had mean participant ages of 62, 58, and 68 years, respectively, whereas the median age for AF diagnosis is 75 years. Thus, direct extrapolation of trial outcomes to older populations must be done cautiously.
Treatment Efficacy and Challenges in Older Adults
Increased Risk Profile
Older adults with AF face elevated risks:
- Falls and Injuries: A Danish registry (2000-2014) of 100,935 elderly AF patients reported a 17% incidence of fall-related injuries and a 5.7% incidence of blackouts within two years. Rhythm-control drugs increased this risk by 29% compared to rate-control drugs, highlighting the need for cautious medication selection.
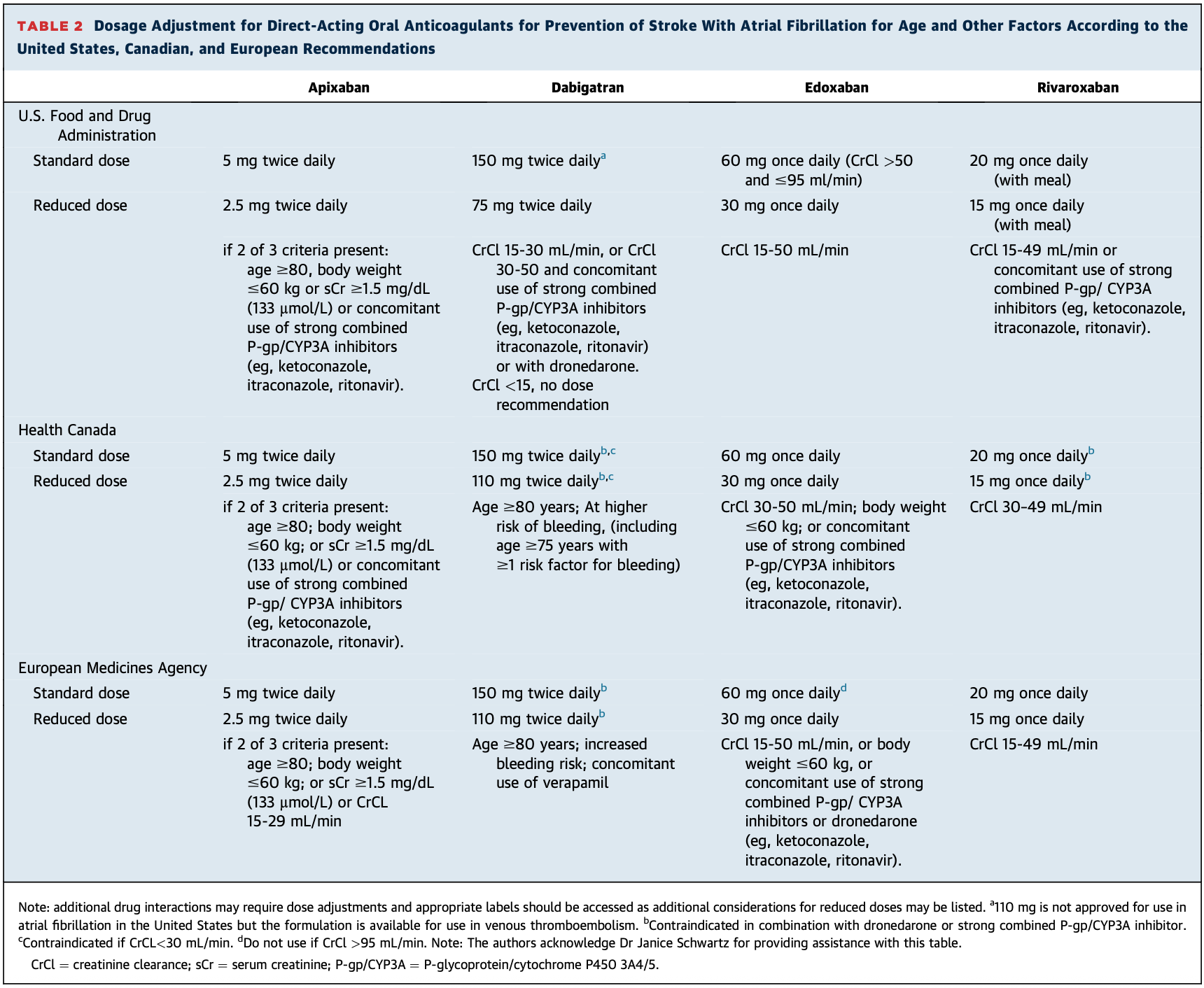
Stroke Risk: is significantly higher, especially when individuals are over 65 necessitating careful anticoagulation management. It becomes even more complicated as dose adjustments may need to be made when individuals are 80 years or older, especially in the context of frailty.
Medication Sensitivity
Medication effectiveness and tolerance decrease unpredictably with age:
- Heart rates naturally slow as we age and this may reduce the required dosage of rate-control drugs (e.g., bisoprolol, verapamil, digoxin).
- Finding stable medication regimens can become challenging in paroxysmal AF in chases where normal sinus rhythm may become excessively slow if AF medications are used.
- Increased prevalence of kidney disease, coronary artery disease, and extensive medication lists complicate drug management and increase interaction risks.
Catheter Ablation in Older Adults
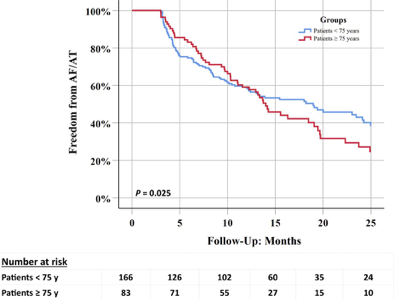
Ablation effectiveness in older adults remains less defined due to limited trial data. Small studies have indicated lower success rates in patients over 75 years compared to younger cohorts.
However, dismissing ablation entirely based on such limited data would be inappropriate:
- Anecdotal evidence and registry data support significant symptomatic improvement and cognitive benefits for selected older patients.
- Individualised assessment remains crucial, with ablation potentially offering considerable benefit to fit older adults.
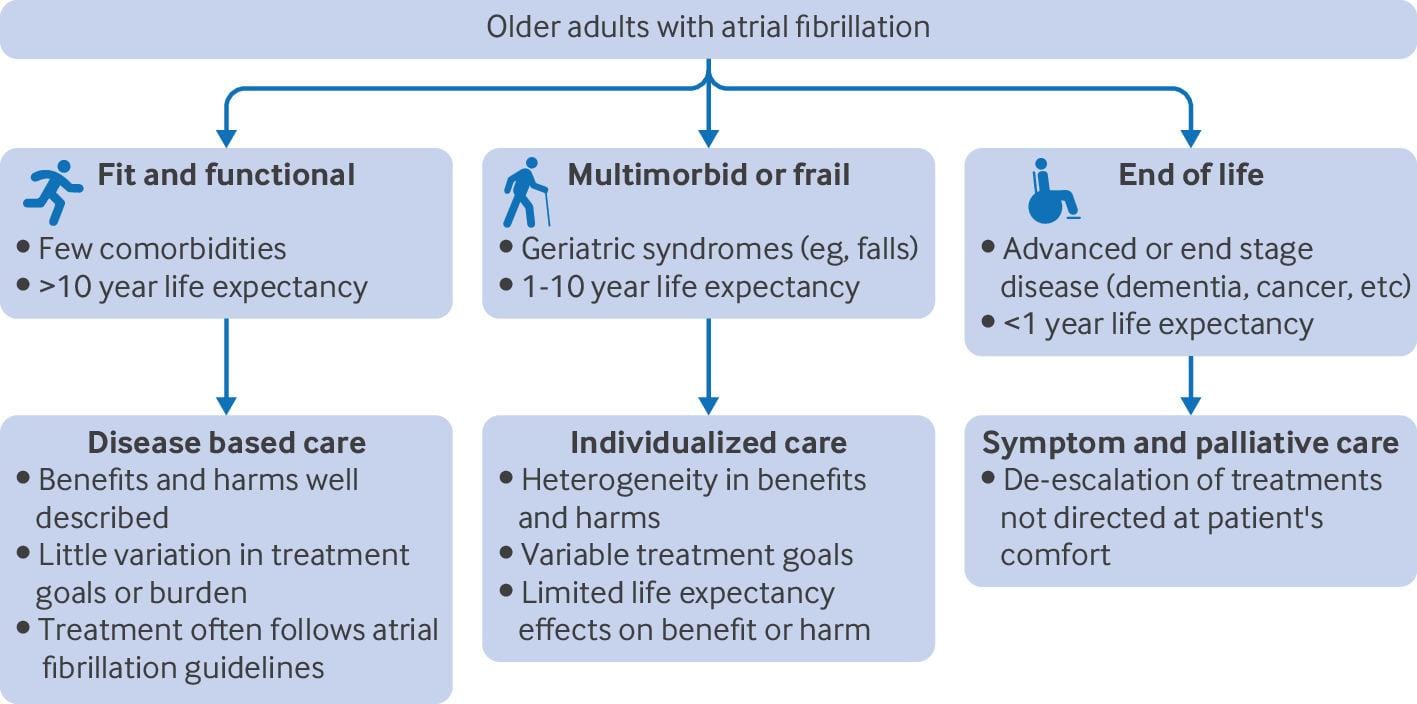
Goal-Directed Care: Personalised AF Management
There is no easy answer to the increased risk and uncertainties around AF management in older adults, but it does reinforce the importance of personalised decision-making. The variability in lived experiences, frailty status and priorities for the future make it incredibly important to consider what the goals of AF treatment should be in the older adult.
- Symptom Management: Prioritising functional status and quality of life over aggressive rhythm control for longer term benefits that take years to accrue.
- Stroke Prevention: Anticoagulation is critical and all patients over 65 years should be offered blood thinners unless there is a strong reason not to.
- Balanced Treatment: Minimising adverse drug effects that effect mobility, energy levels and quality of life is an important factor.
Conclusion
Atrial fibrillation in older adults results largely from age-related cardiac changes and the combination of risk factors that increase with age. Optimal AF management demands a personalised approach balancing stroke prevention, symptom control, and minimisation of treatment risks.
Large screening programmes (to detect AF in undiagnosed people) are being trialled globally and many institute age thresholds- the SAFER trial in Cambridge UK is enrolling almost 100,000 participants across 200 GP practices and uses an age threshold of 70 years or older. The goal is to generate evidence for a potential National screening programme akin to Breast Cancer or Colon Cancer. However, if we are to go searching for undiagnosed AF in these individuals, we need to understand what to do if we find it. Especially as our population continues to age, the demographics of the AF population will continue to be further skewed. Therefore it is important that our research and trials mirror this trend so that we can apply their findings in the real world.